Reduced blood flow to the legs can increase the risk of cramps, especially at night when circulation slows.
Circulation-related cramps may:
-
Occur during rest
-
Improve when standing or walking
-
Be accompanied by cold feet or numbness
Doctors note that circulation problems can also be an early warning sign of vascular disease.
5. Nerve Compression or Irritation
Compressed nerves in the lower back or legs can disrupt signals to the muscles, triggering cramps.
This is more common in people with:
-
Spinal issues
-
Herniated discs
-
Prolonged sitting
Nerve-related cramps may be accompanied by tingling or numbness.
6. Certain Medications
Some medications list muscle cramps as a side effect, including:
-
Diuretics
-
Statins
-
Blood pressure medications
If cramps begin after starting a new medication, it is important to discuss this with a healthcare provider.
7. Pregnancy and Aging
Nighttime leg cramps are especially common during pregnancy and in older adults. Changes in circulation, muscle mass, and nerve function can all contribute.
While often harmless, persistent cramps should still be evaluated.
When Leg Cramps May Signal a Bigger Problem
Although most leg cramps are benign, doctors advise medical evaluation if cramps:
-
Occur frequently
-
Are severe or worsening
-
Affect only one leg
-
Are accompanied by swelling, redness, or warmth
These symptoms may indicate circulation problems, nerve disorders, or blood clots.
What to Do When a Leg Cramp Hits
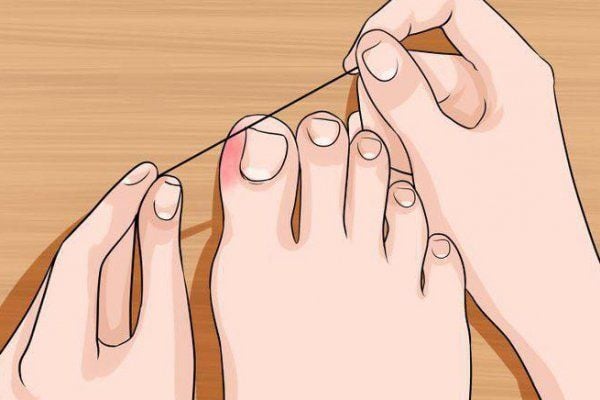
If you wake up with a leg cramp:
-
Gently stretch the affected muscle
-
Flex your foot upward toward your shin
-
Massage the muscle
-
Stand and walk slowly if possible
Applying warmth or a warm towel may help the muscle relax.
The Best Ways to Prevent Nighttime Leg Cramps
1. Stretch Before Bed
Gentle stretching of the calves and thighs before sleep can significantly reduce cramp frequency. Stretching improves muscle flexibility and blood flow.
2. Stay Hydrated
Drink enough water throughout the day, especially if you are physically active or live in a hot climate.
Avoid excessive caffeine or alcohol, which can worsen dehydration.
3. Improve Sleep Position
Sleeping with toes pointed downward can shorten calf muscles. Try:
-
Sleeping on your back
-
Keeping feet in a neutral position
-
Avoiding tight blankets that pull the toes down
4. Wear Supportive Footwear
Shoes that provide proper support during the day reduce muscle strain that can lead to nighttime cramps.
5. Maintain Balanced Nutrition
A diet rich in fruits, vegetables, and whole foods supports electrolyte balance. Supplements should only be taken under medical guidance.
6. Stay Physically Active — But Not Excessive
Regular, moderate activity improves circulation and muscle health. Avoid sudden increases in exercise intensity without proper conditioning.
7. Review Medications
If cramps are frequent, ask your doctor whether medications could be contributing and whether alternatives are available.
When to See a Doctor
Medical professionals recommend evaluation if:
-
Cramps disrupt sleep regularly
-
Home remedies do not help
-
Symptoms are worsening
-
Cramps are accompanied by other leg symptoms
Simple tests can help identify circulation, nerve, or metabolic issues.
Final Thoughts
Nighttime leg cramps are common—but they are not something you simply have to live with. In many cases, small changes in hydration, stretching, activity, and sleep habits can make a big difference.
Most cramps are harmless, but persistent or severe episodes deserve attention. Your body often sends signals before more serious problems develop.
Better sleep starts with listening to those signals.
Don’t ignore what your legs are trying to tell you.